Bacterial memory could be the missing key to beating life threatening pathogens

Sadie Harley
scientific editor

Robert Egan
associate editor
Bacteria aren't just mindless microbes. New research from the Hebrew University of Jerusalem reveals that single bacterial cells can carry a "memory" of their past environments—passing it down through generations—before eventually forgetting.
Using a new technique called Microcolony-seq, scientists uncovered hidden subpopulations inside infections, each with different survival strategies. The finding could explain why antibiotics and vaccines sometimes fail—and may point the way toward more precise treatments.
The discovery, in Cell and led by postdoctoral researcher Dr. Raya Faigenbaum-Romm under the supervision of Prof. Nathalie Q. Balaban, and collaboration with Profs. Ilan Rosenshine and Maskit Bar-Meir, introduces a method called Microcolony-seq that captures microbial memory at the earliest stages of colony growth.
For decades, biologists have known that bacteria—though genetically identical—often behave differently. Some grow fast, some slow; some resist antibiotics while others succumb. But until now, it was unclear which of these differences were fleeting accidents and which represented genuine, heritable states.
"What we found is that even a single bacterium carries a long-lasting memory of where it's been," says Dr. Faigenbaum-Romm. "When it divides, its descendants preserve that memory—sometimes for 20 generations or more."
Microcolonies as a window into memory
The Microcolony-seq method works by isolating tiny colonies that sprout from individual bacteria, analyzing their RNA, genomes, and physical traits. This approach avoids the noise of even recent cutting-edge single-cell RNA sequencing methods, and reveals whether differences between cells are genetic mutations or epigenetically inherited phenotypes.
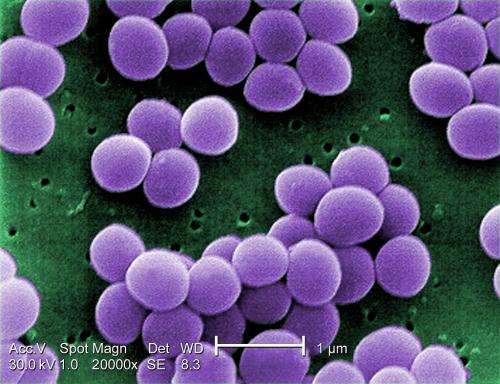
Using this method, the team uncovered surprising stabilities. Pathogens like Escherichia coli and Staphylococcus aureus were shown to split into stable subpopulations—even within a single infection. Some lineages activated virulence programs that help them cling to host cells, while others switched on genes that favored motility or survival in harsh conditions.
Intriguingly, the study showed that this microbial memory has limits. When bacteria reach "stationary phase"—the point when nutrients are depleted—the memory is erased, effectively resetting the population.
Implications for medicine
The discovery carries urgent implications for human health. In urinary tract and bloodstream infections, Microcolony-seq revealed co-existing bacterial subgroups with distinct antibiotic resistance or virulence profiles. A conventional clinical test that samples just one colony could easily miss these hidden players—leading to treatments that fail.
Prof. Balaban explains, "An infection is rarely a uniform population of bacteria. It's more like a coalition of different players, each with its own strengths. To design therapies that truly work, we need to understand—and target—all of them."
This may help explain why so many experimental drugs and vaccines against S. aureus infections have stumbled in clinical trials: they targeted only one part of the bacterial population, leaving others untouched.
Beyond immediate medical relevance, Microcolony-seq opens new avenues for exploring microbial life. It provides a systematic way to study how bacteria diversify, hedge their bets, and adapt in real time. Future applications could extend to fungal pathogens, the gut microbiome, and even industrial fermentation.
As Dr. Faigenbaum-Romm notes, "We've been treating bacteria as if they're all the same, but in reality, even a single cell carries a story of its past. Microcolony-seq lets us finally read that story."
More information: Uncovering Phenotypic Inheritance from Single-Cells with Microcolony-seq, Cell (2025). .
Journal information: Cell
Provided by Hebrew University of Jerusalem




















